What You Should Know About Blood Clot Prevention.
Blood clots are dangerous diseases that require special attention. The
condition is one of the leading causes of death and disability worldwide.
Statistics show that there are 900,000 blood clots yearly in the United States,
of which 100,000 die annually. The American National Blood Clot Alliance states
that the total number of deaths from blood clots is far much significant than
the number of people who lose their lives to AIDS, breast cancer, and
automobile accidents yearly.
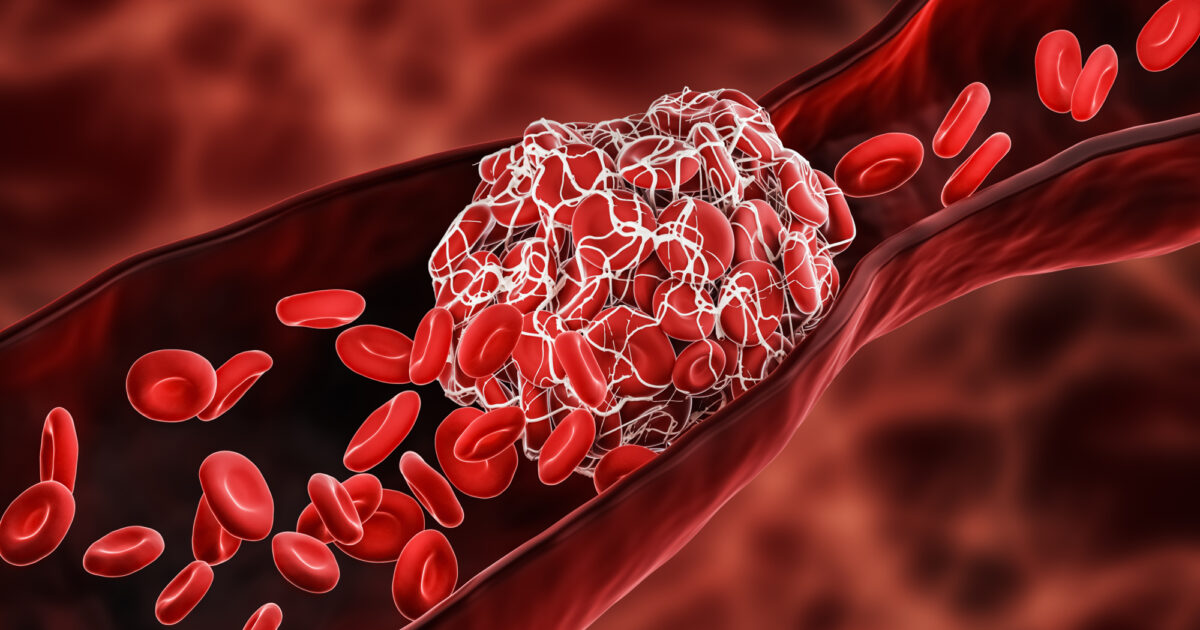
The Cleveland Clinic defines
blood clots as jelly-like collections of blood that form in veins or arteries
when blood goes from liquid to partially solid. When blood forms in your reins,
it can cause serious health problems. These blood clots can break off, go
through your body and block blood flow to your organs. When a blood clot takes
place where it shouldn't have, it is called a thrombus. A blood clot is further
called a thrombus. When the clot stays in one place, it's called thrombosis,
and when it moves through the body, it's called an embolism or thromboembolism.
Occurrence
Blood clots can occur in the
abdomen, arms, legs, brain, heart, and lungs. Venous thromboembolism (VTE) can
be divided into two parts: deep vein thrombosis (DVT) ( clot may occur in a
deep vein, an arm or leg), and pulmonary embolism (PE), a lump already broken
off and entered the lungs.
Signs
All body parts with a blood
supply are vulnerable to blood clots. Symptoms will vary depending on where the
clot blocks blood flow. Some signs include warmth, swelling, pain, or
tenderness unrelated to an injury, particularly in one or both legs, a
discolouration (redness or blueness) of the skin on your legs, and sudden
trouble breathing or shortness of breath. Other symptoms include fast, erratic,
or irregular heartbeat, chest pain, dizziness or fainting, low blood pressure,
significantly if pain worsens with coughing or deep breathing, and coughing up
blood.
Anyone, irrespective of age, can
get blood clots, especially deep-vein thrombosis (DVT); adults over 60 and
hospital patients are more likely to develop this condition. The human body
responds to an injury or cut by adequately clotting blood. This type of blood
clot is not dangerous. A blood clot can form without it being caused (for
example, by an injury or a cut). Certain risk factors or conditions make this
more likely.
Risk Factors
The following risk factors are
obesity, pregnancy, immobility including prolonged inactivity, long journeys,
smoking, oral contraceptives, certain types of cancer, trauma, certain
surgeries, age (higher risk for those over 60 years), a family history of blood
clots, chronic inflammatory diseases, diabetes, high blood pressure, high
cholesterol and earlier placement of a central line.
Other Diseases
Some diseases and health conditions
can increase an individual's risk of developing blood clots. Conditions include
cancer, COVID-19, and heart conditions such as congestive heart failure,
atherosclerosis, and hypertension.
Others include chronic kidney
disease, blood disorders, inflammatory bowel disease, Behcets disease,
rheumatoid arthritis, systemic lupus erythematosus, asthma, sepsis, obstructive
sleep apnea, tuberculosis, diabetes, and polycystic ovary syndrome.
Medical Test
Since there are other conditions
with symptoms similar to blood clots, special tests are needed to diagnose a
blood clot, which can look for lumps in the veins or lungs (imaging tests).
Your doctor may recommend the following medical examinations: blood tests and
ultrasound, which give a better view of your veins and blood flow. Others are
CT scan of the chest, abdomen, or head, magnetic resonance angiography (MRA),
and V/Q scan Test circulation of air and blood in the lungs.
Medications and
Treatments
When a blood clot is diagnosed,
your general health and where you have the blood clot will determine treatment
options. Your doctor may recommend medications such as anticoagulants, which
prevent blood clots, and thrombolytics. The latter can destroy blood clots that
have already formed. Compression stockings also apply pressure to reduce leg
swelling or prevent blood clots from forming. Other treatments include stents,
which are known to keep blood vessels open, vena cava filters that prevent
blood clots before they can get to the lungs, and surgery.
Scientists and medical experts
have recommended natural ways and lifestyle changes that can reduce your risk
of getting blood clots. Changes include:
Regular exercise. Since physically inactive lifestyles have been linked to blood clots,
it is advised that you walk for not less than 30 minutes per day to maintain
your circulation.
Drink water. You can prevent blood clots by drinking plenty of water daily, not
less than eight glasses daily.
Walk. Pregnant women should take regular walks. Blood clots can occur due to
the hormonal changes brought on by pregnancy, so it's crucial to keep your leg
muscles contracting to help blood flow when you walk.
Weight. Maintain a healthy weight. Blood clots can form due to weight gain and
the increased venous pressure that comes with carrying extra pounds. Weight
loss and a healthy weight can lower your risk of clotting.
Take a break. Break long sedentary periods of travel, illness, or your job demands you
to sit for long periods; you must stand up and move around often. To prevent a
clot from forming, the Centers for Disease Control and Prevention recommends
standing, stretching (feet, ankles, and legs), and moving about every 2 to 3
hours if possible.
Avoid smoking. If you smoke, it's high time you quit. According to research,
medical experts have discovered that smoking increases the risk of developing a
dangerous blood clot.
Although no one is immune to
blood clots, it's wise to look for signs of blood clots and contact your doctor
as soon as you suspect something is wrong.
Photo: Heart Research Institute https://www.hri.org.au/